Osgood-Schlatter Disease
What Is Osgood-Schlatter Disease?
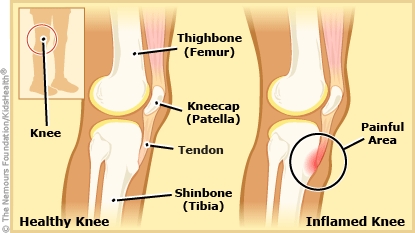
Osgood-Schlatter disease (OSD) is swelling and irritation of the growth plate at the top of the shinbone. A growth plate is a layer of cartilage near the end of a bone where most of the bone's growth happens. It is weaker and more at risk for injury than the rest of the bone.
OSD goes away when a person stops growing and usually doesn't cause lasting problems.
What Are the Signs & Symptoms of Osgood-Schlatter Disease?
OSD typically causes pain and swelling below the kneecap. The pain usually gets worse with running, jumping, going up stairs, and walking up hills. Severe pain may lead to limping. OSD can happen in one or both knees.
What Causes Osgood-Schlatter Disease?
Osgood-Schlatter disease happens during the growth spurt of puberty, when the bones, muscles, and tendons grow at different rates. In OSD, the tendon that connects the shinbone to the kneecap pulls on the growth plate at the top of the shinbone. Activities and sports cause this to happen over and over, which causes injury to the growth plate. This injury leads to the pain of OSD.
Who Gets Osgood-Schlatter Disease?
OSD usually happens in kids and teens who are:
- in their growth spurt (usually around 9–14 years old)
- active in sports or activities that involve a lot of running or jumping
OSD is an overuse injury. This means it happens when someone does the same movements over and over again.
How Is Osgood-Schlatter Disease Diagnosed?
To diagnose Osgood-Schlatter disease, health care providers:
- ask about physical activities
- do an exam
Usually no testing is needed. Sometimes the health care provider orders an X-ray to check for other knee problems.
How Is Osgood-Schlatter Disease Treated?
Someone with Osgood-Schlatter disease needs to limit activities that cause pain that makes it hard to do that activity. For example, if you feel a little pain when running it's OK to keep running. But if running causes a limp, stop and rest. When the pain is better (usually after a day or two), you can try the activity again.
Sometimes health care providers recommend physical therapy (PT) to keep leg muscles strong and flexible while you get better. It doesn't happen often, but some teens might need a total break from all sports and physical activities.
To feel more comfortable while healing from OSD:
- Put ice or a cold pack on the knee every 1–2 hours for 15 minutes at a time. Put a thin towel between the ice and your skin to protect it from the cold.
- If your health care provider says it's OK, you can take ibuprofen (Advil, Motrin, or store brand) or acetaminophen (Tylenol or store brand). Follow the directions that come with the medicine for how much to take and how often.
How Long Does Osgood-Schlatter Disease Last?
Osgood-Schlatter disease usually goes away when the bones stop growing. Typically, this is when a teen is between 14 and 18 years old.
Can Teens With Osgood-Schlatter Disease Still Do Sports?
Yes, teens with OSD can usually do their normal activities, including sports, as long as:
- The pain is not bad enough to interfere with the activity.
- The pain gets better within 1 day with rest.
If you play sports, it can help to:
- Wear shock-absorbing insoles in your sneakers and cleats.
- Put a heating pad or warm washcloth on the knee for 15 minutes before sports.
- Put ice on the knee for 15 minutes after the activity (with a towel between the ice and the skin).
- Wear protective kneepads, especially for wrestling, basketball, and volleyball.
- Stretch before and after sports.
Looking Ahead
Long-term effects of OSD usually aren't serious. Some teens may have a painless bump below the knee that doesn't go away. Very rarely, doctors will do surgery to remove a painful bump below the knee.
Some adults who had OSD as kids or teens have some pain with kneeling. If you still have knee pain after your bones stop growing, see your health care provider. The provider can check for other causes of knee pain.
